AHW Day #1 Recap
If you haven’t been to an Australian Healthcare Week before – it’s a full smorgasbord board of all things Healthcare. There is a lot of ground to cover and it is not possible to do it all justice here. But we’ve pulled together some insights from the presentations and vendors we visited.
Thanks to everyone who gave us time and answered our multiple questions throughout the day – see you for day 2.

The Missing Link: The Need for Our Strengthening Medicare Taskforce Report to Address Our Burgeoning Workforce Crisis
The Honourable Senator Anne Ruston
Shadow Minister for Health and Aged Care
For anyone in health it will be no surprise that workforce issues are high on the list of challenges currently. Finding, hiring, training and retaining staff (and keeping them well) featured strongly.
The honourable senator discussed how Access to workforce is a critical challenge and that sustainable staff models are not necessary about cutting costs but rather investing in the tools, systems and people that deliver outcomes – this may be more expensive than current traditional models.
Equity and access to regional healthcare is also at a critical juncture – regional training pathways and clinicians are in need and must be ably supported by digital technology and metro based sub specialties. These approaches must be aligned to the nuanced needs of each region.
In terms of increasing the number of staff. International Medical Graduates and fast tracking visa’s were highlighted but seemingly are only a short term solution.
The Senator also suggested there is still some spending waste in the healthcare budget particularly at the nexus between federal and state responsibilities. Are our clinical settings driving outcomes and quick adoption and innovation in new models of collaborative care? We think in patches.

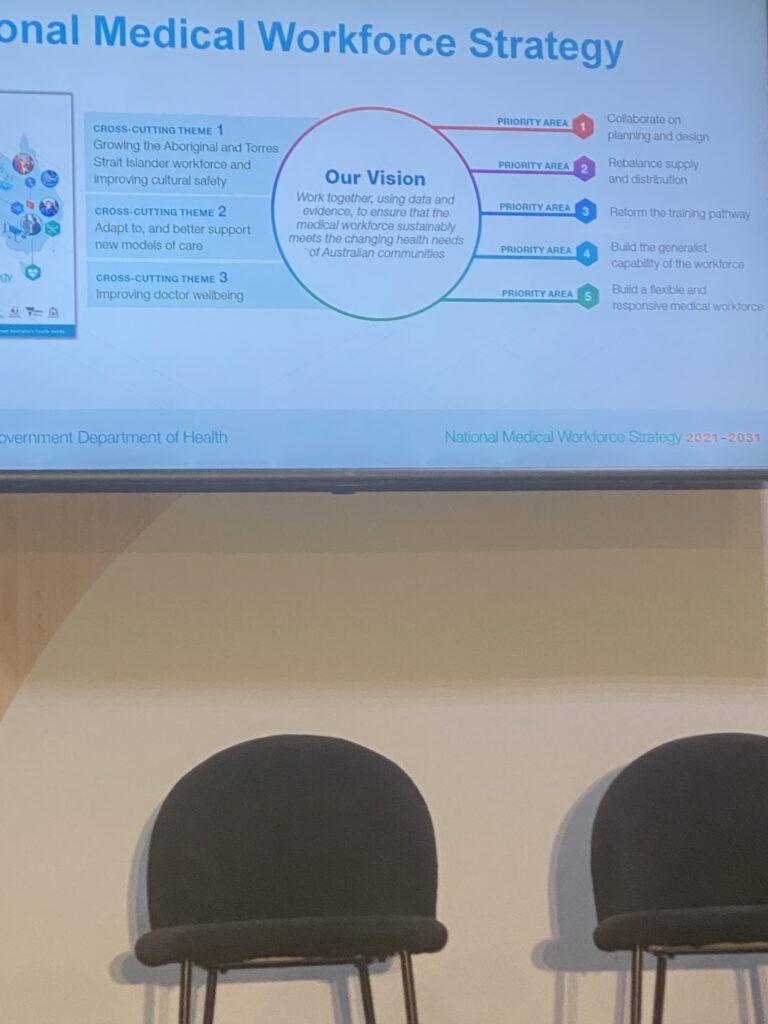
Unpacking The Practical Challenges with Bringing The 10 Year National Medical Workforce Strategy to Life
A / Prof Susan Wearne
Senior Medical Advisor, Health Workforce Division Australia Department of Health & Aged Care
Prof Wearne offered an informative session on the currently 10 year strategy for the Medical workforce nationally. You can read the full report here
The approach the Health Workforce Division has taken was to focus on Medical changes / improvements and the ‘dollars will flow’ with it.
There was some interesting and challenging information presented. Particularly relating to challenges around Culture and safety issues for training doctors, the high number of unaccredited trainees (~5,500), the low and dropping numbers of GPs (particularly in regional and rural areas) and the impact of fractured datasets in completing robust future workforce planning. In addition International medical graduates and training locums and unaccredited trainees clinical governance challenges as all professions (not just medicine) free clinical staff up to work at the top of their scope of practice.
The lack of comprehensive data on collective workforce numbers (and to a degree associated models of care) was
The prediction that there would be no ‘interesting’ jobs for doctors to do, won’t become reality until funding and remuneration for ‘less interesting’ medical jobs change.
Slow progress and implementation of solutions is expected and engagement with the team particularly around sharing workforce datasets was encouraged.
Think Tank: Getting Creative – The Role of Alternate Workforces, Data & New Care Models in Solving Our Workforce Planning Challenges
Analytics is going to be critical in current and future workforce planning, particularly when trying to address challenges like a doubling of non practicing nursing registrations.
Despite there being an identified need to leverage predictive analytics, simulation modeling and even AI in planning and managing the workforce, poor data quality and fragmented systems plague health. Despite healthcare workers having banking and other information shared in various formats e.g. social media and in some cases multiple locum agencies there is a concern about privacy. Perhaps we’re getting personal health information and general registration and education information confused in this situation.
Having a data manager vs a culture of tech literacy and data quality. The old rubbish in, rubbish out reared its head here. Both arguments make sense in a way. Have a data manager on each ward who is perpetually responsible for reporting, analytics and communicating outcomes so clinicians can work at the top of their scope of practice and be informed by the information presented. Alternatively, the clinicians take some extra time during their administration of patient notes, etc. to ensure the fullness and quality of the information going into various systems putting strain on their ability to work at full capacity.
The Alpha generation as grown up attached to devices is expecting more from health systems. Easy access to information, support and ability to enable their careers from mobile devices is key. There is already a push in some states and facilities to enable common sense use of personal mobile devices for non patient related work activities and in some cases, where appropriate this clinical use. Everyone needs to move forward with technology. Hopefully legal and the decision makers can keep up.
Learning from excellence – An excellent comment from Mary Chiarella – we’re doing a lot of learning from errors and catastrophe (and rightly so), but not a huge amount of learning from (and celebrating of) excellence – where are the M&Ms on when things go well?
The conversations closed with an interesting take of workforce plans. Like most plans, they rarely survive the first contact. Variation in approach and measurement make it almost impossible to determine the effectiveness of the planning process. A central theme was plans we’re putting more weight on the financial needs of the organisations vs building and supporting staffing models that enable care. To go hand in hand, but ultimately a financial decision needs to be made.
MDOK: How Australia’s first Wellbeing Centre’s Is Operationalizing a Data-Driven Approach to Its Wellbeing Program to Improve Impact Across 15,000+ Staff
Dr Bethan Richards from SLHD the first Chief Wellness officer – who over the last five years has slowly but surely built a successful wellbeing culture across Medicine, that will soon be expanded across all staff in Sydney Local Health District.
The key takeaway I tool from the presentation:
- Focus on the drivers of distress. One size does not fit all in your solutions, data needs to inform your decisions on actions and initiatives. DON’T LEAD WITH YOGA
- Target interventions to your cohorts e.g. Theatre staff will need different solutions that Emergency staff
- Change the narrative around your EAP – it is about being at your best, not somewhere to turn to when you’re at your limit. Having your EAP reps involved in orientation and training sessions to reinforce this message.
- Excellent to see the program has led to a decrease in safety issues.
- Data and evidence is critical to show you are making a difference both for staff and executives to encourage reinvestment. There is and should be a shared responsibility between the executive and the frontline staff. Participate fully in supporting and engaging with the program. Likewise wellness needs to be included in Strategic plans, talked about in executive and middle management meetings alike.
- The 5% rule – each initiative will only impact 5% of staff – so there will need to be a few things happening
There is a growing body of evidence around clinician wellbeing. Each organisation should be prioritising these strategies and planning a long game. You can’t run resilience training and everyone be resilient.
Our own Dr Cailtin Weston did a Churchill fellowship on Burnout and Wellbeing – you can find it here.
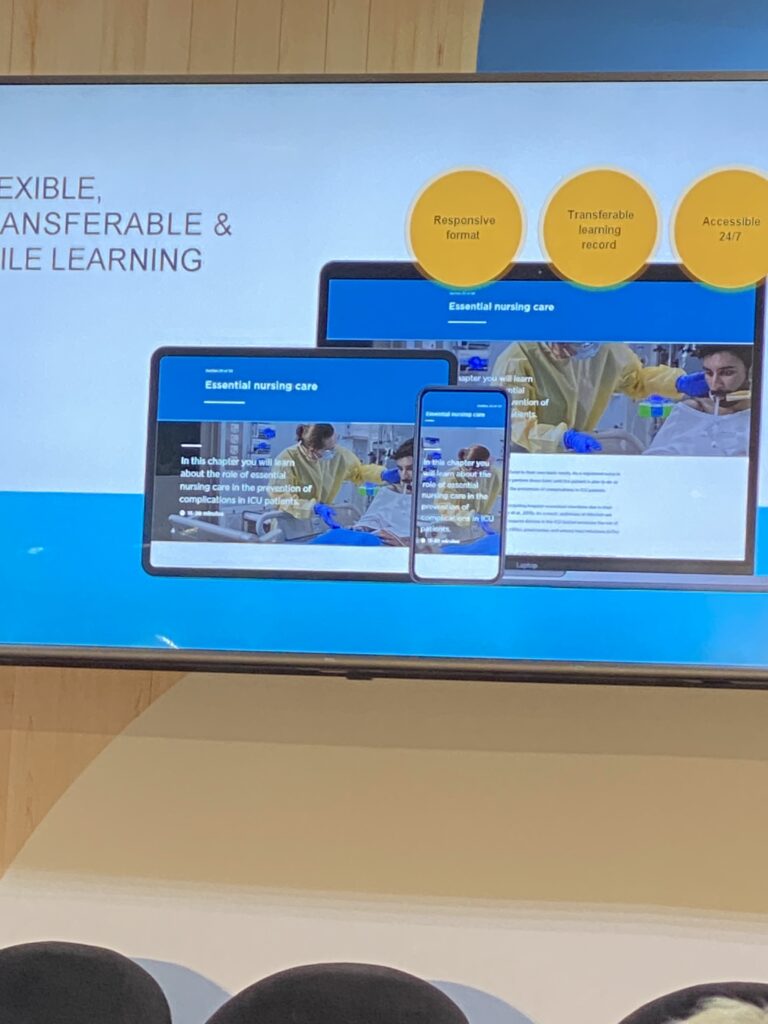
How We Can Bring Agility to Staff Education to Address Skill Shortages and Meet the Dynamic Capability Needs of Our Health System
HETI
Great to see some updates out of HETI, NSW on their war on paper and focus on improving the learning experience for staff, in particular the clinical staff. The Transition to ICU Nursing pathway was a great example of this. Removing all paper based workbooks, providing short, sharp point of care learning was available with learning outcomes linked to relevant quality, safety and nursing standards.





Thanks for the comprehensive recap Tom. What a future healthcare is facing!