Case Study
Nursing Quality Improvement
Challenge
In 2022, A New South Wales Local Health District in metropolitan Sydney identified that the incidence of falls had been increasing during the COVID-19 pandemic. The falls were not specifically limited to aged care wards or Geriatric patients in the district. While inpatient falls are often multifactorial, the impact of COVID-19 on the delivery of care created additional risk factors:
- Increase in patient acuity
- PPE requirements for staff
- Increase in older patients treated outside of specialist units
- Remoteness of monitoring
- Increase in agency / short-term staff
With the average cost of inpatient falls upwards of $7000¹ (falls resulting in complex injuries such as a fractured Neck of Femur or intracranial haemorrhage have an average additional 18.8 days LOS with $38,991²) the LHD wanted to use Med App to pilot a quality improvement activity around falls prevention.
Solution
A quality activity was collaboratively designed by district stakeholders and the Med App Hospital Success Team. As inpatient falls are multifactorial and have multiple variables, the focus of the quality improvement project was the staff experience. A reduction in falls rate was considered a benefit of this initiative but not a main objective.
Harnessing the capabilities and features of Med App, the pilot aimed to:
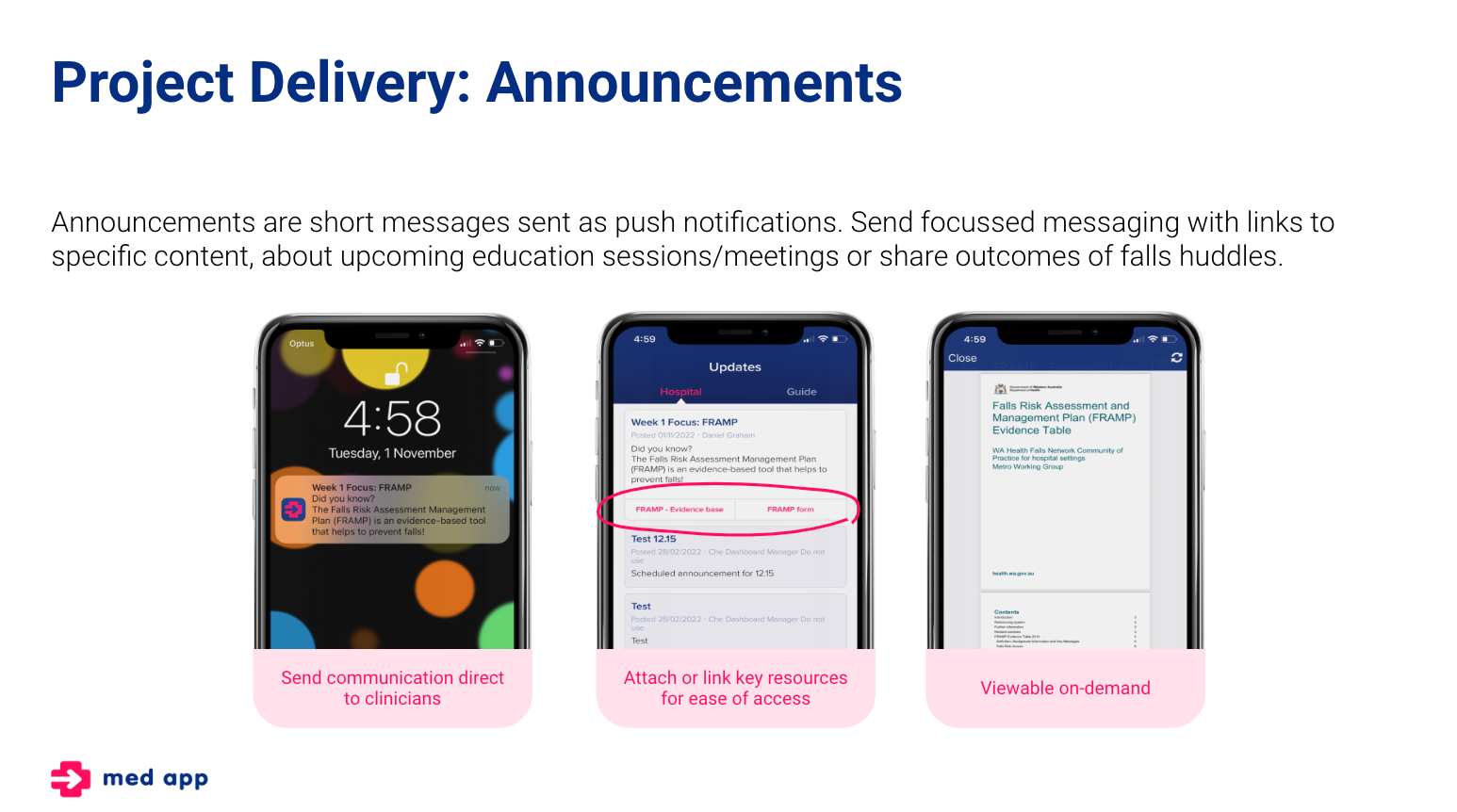
Increase staff awareness of available Falls clinical and educational content in Med App
Increase engagement with Falls prevention and harm minimisation through specific comms
Improve general ward communication about Falls
Improve staff confidence in preventing and managing falls
Increase accessibility to falls information
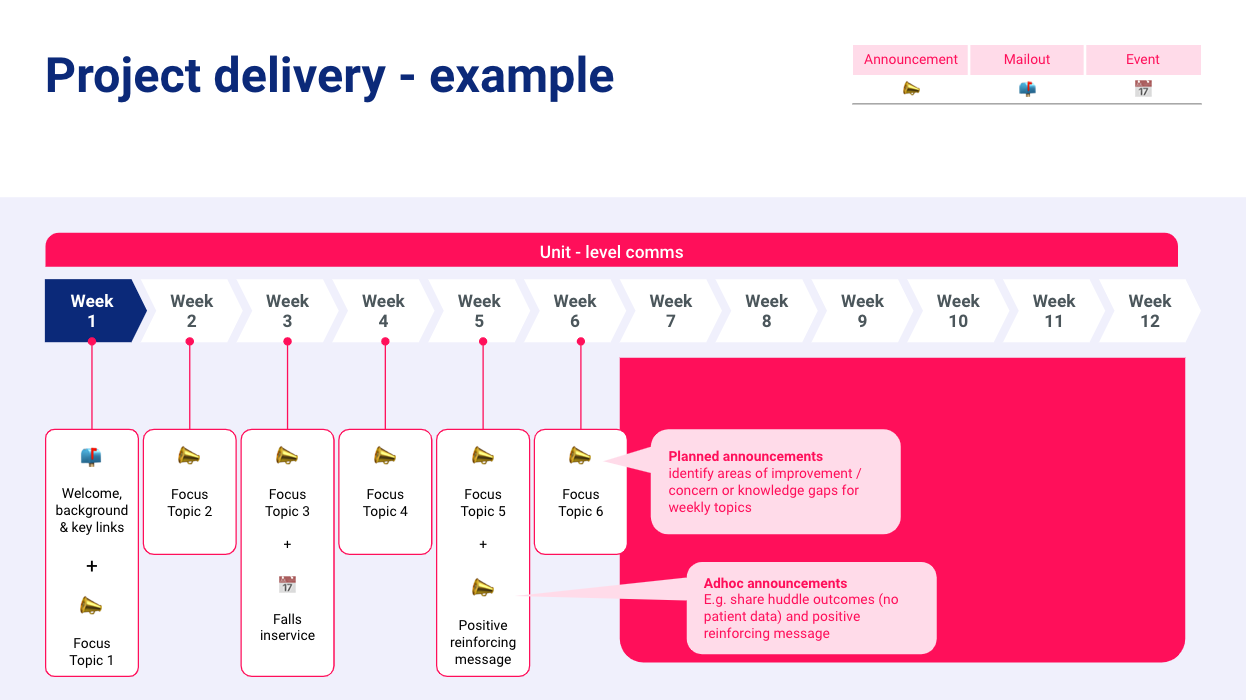
Five wards across four hospitals took part in the pilot over 12 weeks. All staff working on the participating units (nursing, medical and allied health) were invited. Falls content was uploaded/linked to Med App by the district Falls Coordinator in preparation for the project. The content could be accessed freely by staff and was utilised as specific links in the Falls comms sent out to staff.
Key Outcomes
- At the end of the pilot, their falls rate = 4 for the final month (55% lower than their 12-month average of 9).
- Using their 12-month average, the projected savings for the ward is $420,000 if the project was continued over 12 months.
- The facility had an 12-month average of 5 falls per month across 17 clinical areas. Reducing the falls rate by 1 fall per ward (17) over 12 months would be a saving of $1.4m.
Evaluation staff surveys found the following outcomes
- Staff felt more confident (or at least, the same level of confidence) since implementation.
- 60% of respondents felt more confident with Conducting a falls risk assessment (OMS) and completing a Falls Risk Management Plan.
- Staff reported an overwhelming improvement in ease of access.
- Some items showed significant improvement e.g. the Falls referral pathways were easier to find (100% respondents).
- Resources/information easily accessible at the point of patient care, making it very convenient to use – navigating intranet to locate relevant resources can be time consuming.
- Weekly focus topics provided both a refresher as well as some new learnings, even for experienced staff on the ward.
- Additional announcements acknowledging the sustained reduction in monthly falls rate throughout the pilot project were meaningful, supportive and motivating – staff reported that the feedback felt more personal than when it is presented in other forums such as ward meetings.
%
Reduction in Falls
%
Increase in staff confidence
Key Learning & Opportunities
Lessons learned included the need to conduct a thorough readiness assessment - two of the participant wards were preparing for a move to a newly built building which took precedence over locally leading the falls QI project.
Messaging about content alone has limited impact - tying the messaging in with inservices/education sessions and adhoc messaging to share outcomes of falls huddles, falls data, positive reinforcement yields a much stronger result through more meaningful engagement with the app.
Messaging for some of the wards was generic - having a personalised touch from the ward leadership teams could help to address pain points more effectively and specifically.
Further testing should be conducted in other units/contexts to replicate and validate findings.
References
- Morello, R, Barker, A, Watts, J, Haines, T. et al. 2015. ‘The extra resource burden of in-hospital falls: A cost of falls study’, Medical Journal of Australia, vol. 203, no. 9, pp. 367..
- Australian Commission on Safety & Quality in Healthcare 2018. ‘Hospital-Acquired Complication 2: Falls Resulting in Fracture or Intracranial Injury, online, https://www.safetyandquality.gov.au/sites/default/files/migrated/Falls-resulting-in-fracture-of-intracranial-injury-detailed-fact-sheet.pdf
Download Case Study
Simply enter your details below and click download to get a copy of the case study.

