If you’re a junior doctor who doesn’t see the need, have the inclination, or even know how to get involved in medical leadership, I can totally relate.
Not so long ago, I was that kind of junior doctor too.
Never really a joiner, I didn’t participate in my high school student council or university medical student society. Nor was I part of the Resident Medical Officer (RMO) society when I started working in hospitals. My rationale was that someone else was taking care of ‘it’. Besides, I just wanted to be a good clinician (surely that was enough?) and I definitely wanted to stay away from the politics.
That is, until something changed.
The frustrations with limited access to useful clinical resources, messy handovers, poor orientations, disenfranchised staff, and the impact it was all having on my vulnerable patients reached a boiling point where I realised that I could either be part of the problem or the solution. I opted for the latter.
We’re all aware existing systems have the potential to harm patients. Famous studies from America noted estimation of 44,000 to 98,000 deaths per year from medical errors1,2 as the ground-breaking Quality in Australian Health Care Study, published in The Medical Journal of Australia, reported that 16% of patients in hospitals experienced some form of adverse event during their admission and approximately 50% of these were preventable3. These figures alone are concerning enough, but doing nothing is more of a worry.
Inspired by Atul Gawande, I signed up to a systems improvement hospital program in Western Australia (WA). This prompted me to see the possibilities and change from clinical training to join the Royal Australasian College of Medical Administration (RACMA) and galvanised my belief around the urgency and imperative for junior doctors to be involved in medical leadership.
Now with experience of ‘getting involved’ – and research to back my decision – here are three reasons you should get involved too.
#1 – [Junior] Doctors must lead the change
Cynics may laugh, but there is no doubt doctors must lead change from the inside out.
And junior doctors are key to this evolution.
Why? Just consider the statistics around junior doctor mental health issues, medical engagement, and patient safety.
Here’s what else the research tells us:
- Clinician engagement is essential to achieving better patient outcomes as improved engagement in a healthcare organization is known to impact positively on clinical outcomes4.
- Failure to engage junior doctors can have negative impacts on safe, efficient, and effective patient care5.
- Distressed and unwell doctors have higher rates of attrition and decreased rates of workplace efficiency and productivity6.
- Poor junior doctor health has been shown to impact negatively on patient outcomes, including medication errors, clinical performance, and patient experience 7,8.
- Conversely, positive job satisfaction has been shown to improve workplace performance, decrease burnout and improve engagement between the workforce and the organization, improving retention, productivity, and overall patient safety 9,10.
- Junior doctors involved in systems improvement initiatives have been linked to improved aspects of clinical retention, organizational culture, patient engagement, and sustainable, cost effective clinical outcomes 11,12.
These research findings are compelling and provide a strong basis for getting involved. And while junior doctors may think it’s difficult to find a spot on an organisation’s financially constrained agenda already crammed with goals to meet national targets, this is where advocacy for junior doctors’ needs can be addressed by those charged with that responsibility.
What’s the take away?
Use the outlets available to you as a junior medical officer. Have your say through the unit satisfaction surveys sent out by your Medical Education Unit and by contacting the Director of Clinical Training or Medical Administration Registrar. The Junior Doctor Society is always a good place to start and I’ve known quite a few Medical Directors who would love to have a coffee chat about new and innovative ideas.
#2 – Don’t give up: It’s an opportunity to demonstrate medical leadership
I learned very quickly the intention to do good is not necessarily welcomed by all. In fact, expecting resistance is more realistic.
When I moved to Australia as a junior doctor and realized my hospital didn’t have a “common calls” handbook, I made one and gave it to the medical education unit (MEU). Despite initial concerns about maintenance and governance, it ended up being evaluated as the most useful resource for junior doctors.
Similarly, a group of junior doctors attempted to establish a peer mentoring program. Faced with resistance, we set it up as a research project, ran a pilot, proved the program’s value and now distribute resources to other organisations to help start their own.
What’s the take away?
Neither outcome would have been achievable without the help and involvement of junior doctors prepared to step into a medical leadership role.
By its very nature, leadership requires courage and a willingness to persist, so if you decide to get involved, don’t give up at the first sign of resistance. Instead, find an ally or two. Work together and find solidarity in supporting, debriefing, and mentoring each other.
#3 Getting involved opens up opportunities
It’s so easy to give up when the going gets a little tough.
Being a junior doctor is hard enough without the challenges that arise when you develop your medical leadership ‘muscle’. I know, because there have been times when I felt it was all too overwhelming. But here’s the thing: Change starts with a mindset, and once you gain momentum by taking action, opportunities emerge.
Practically, getting active means:
- Brainstorm ideas with your fellow multidisciplinary clinicians, the education team, or even the Medical Director.
- Taking steps to transform the RMO society to a vehicle for change rather than a way to pad your CV.
- Build your skills through communications and project management workshops.
- Take the initiative and sign up to lead projects.
- Consider training with RACMA – this opened the door to meet incredible like minded people, learn new skills, and build on career opportunities
In recent years I have enjoyed the opportunity to change the way doctors and nurses work in meaningful ways. My quality improvement projects have been as diverse as creating after hours survival guides, improving orientations and handovers, implementing an electronic task management system after hours, empowering JMOs through hospital forums and leadership terms, and rolling out peer mentoring program resources across Australia.
It’s not always going to be smooth sailing, but with each success, my enthusiasm grows and I’m confident that yours will too.
What’s the take away?
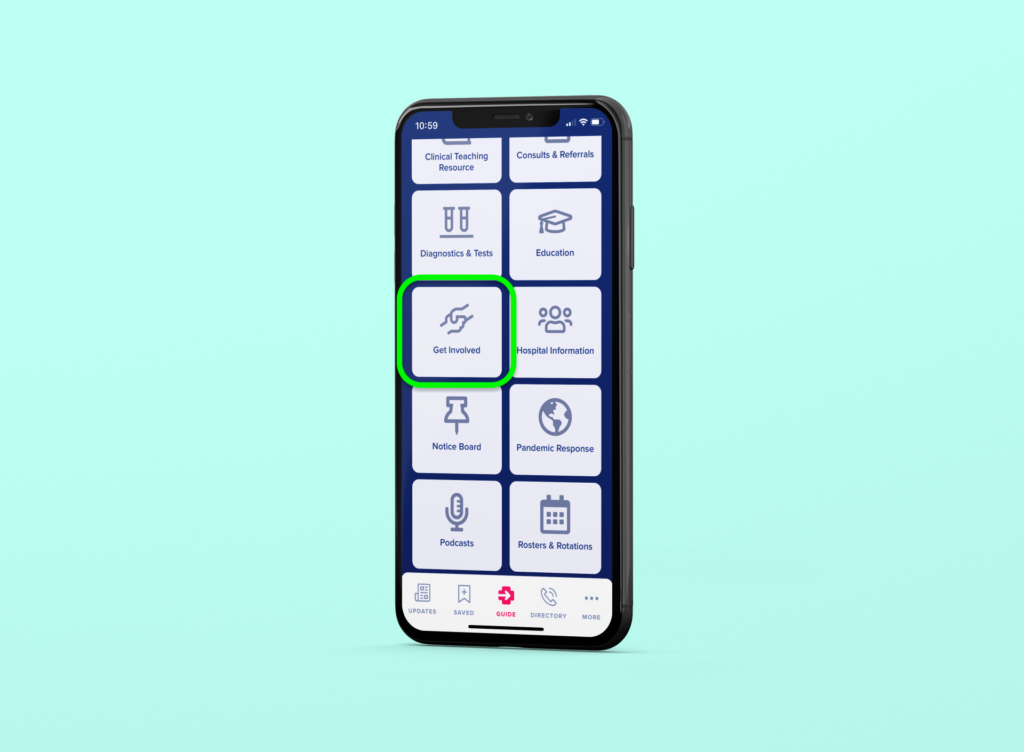
Remember, it’s your hospital too so it’s important to be involved from day one. Your fresh eyes can help others to see things differently. Have an idea or are looking for inspiration? There are free resources available through mobile apps like Med App.
A final word
I now have a natural bias towards encouraging junior doctors to get involved in quality improvement projects, but remember, that wasn’t always the case with me. What I can now say with confidence is that the rewards far outweigh the drawbacks – and I’m certain that as an emerging JMO leader, you’ll make this discovery yourself.
Looking for ways to get involved or after tools and strategies to implement quality improvement projects? Med App* can help. As a free offline-first downloadable app designed especially to support junior doctors and the health professionals they work with, Med App provides an extensive library of resources for getting involved, including JMO leadership courses, access peer mentoring resources, quality improvement toolkits, and more. Still have questions? Connect with Dr Sonia Chanchlani, Med App’s Chief Medical Officer via email at [email protected], or uncover the possibilities when you book a complimentary Med App demonstration.
*Available on the App Store for iOs and Google Play for Android.
- Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. New England journal of medicine. 1991 Feb 7;324(6):370-6.
- Thomas EJ, Studdert DM, Newhouse JP, Zbar BI, Howard KM, Williams EJ, Brennan TA. Costs of medical injuries in Utah and Colorado. Inquiry. 1999 Oct 1:255-64.
- Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Medical journal of Australia. 1995 Nov;163(9):458-71.
- Spurgeon, Peter, Patti M. Mazelan, and Fred Barwell. Medical engagement: a crucial underpinning to organizational performance. Health Services Management Research 24.3 (2011): 114-120.
- Keogh, B. 2009. A junior doctor’s guide to the NHS. In: MCCAY, L. (ed.). London: BMJ Group.
- Wallace, Jean E., Jane B. Lemaire, and William A. Ghali. Physician wellness: a missing quality indicator. The Lancet 374.9702 (2009): 1714-1721.
- Shanafelt, Tait D., et al. Burnout and self-reported patient care in an internal medicine residency program. Annals of internal medicine 136.5 (2002): 358-367.
- Fahrenkopf, Amy M., et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 336.7642 (2008): 488-491.
- Hamilton, P., Spurgeon, P., Clark, J. et al. 2008. Engaging doctors: can doctors influence organisational performance. Coventry: NHS Institute for Innovation and Improvement CNHS Institute for Innovation and Improvement.
- West, M., Dawson, J. 2012. Employee engagement and NHS performance. The King’s Fund, 1-23.
- Dickson, Graham, et al. “Developing junior doctors as leaders of service improvement.” Leadership in Health Services (2014).
- Health Workforce Australia. 2013. Health LEADS Australia: The Australian Health Leadership Framework. Canberra: Health Workforce Australia.




0 Comments